EMDR for ADHD
Jan 14th 2026
ADHD is a neurodevelopmental condition, not a trauma disorder.
EMDR was designed to treat trauma, not attention deficits.
So why is EMDR for ADHD even being discussed?
Because many people with ADHD don’t just struggle with focus — they struggle with chronic emotional dysregulation, shame, rejection sensitivity, and stress overload, often rooted in adverse life experiences. EMDR doesn’t change ADHD’s core neurobiology, but it may reduce the emotional burdens that make ADHD significantly harder to manage.
This guide separates hope from hype, theory from evidence, and what EMDR can help from what it clearly cannot — using current research, clinical consensus, and responsible boundaries.
What ADHD Is — and Is Not
ADHD is a neurodevelopmental disorder characterized by differences in brain development and function, particularly in networks involved in executive control and motivation, as defined in the DSM-5-TR (American Psychiatric Association).
Core neurobiological features include:
- Executive function impairment (planning, task initiation, organization)
- Dopamine regulation differences affecting motivation and reward
- Working memory limitations
- Inhibitory control challenges
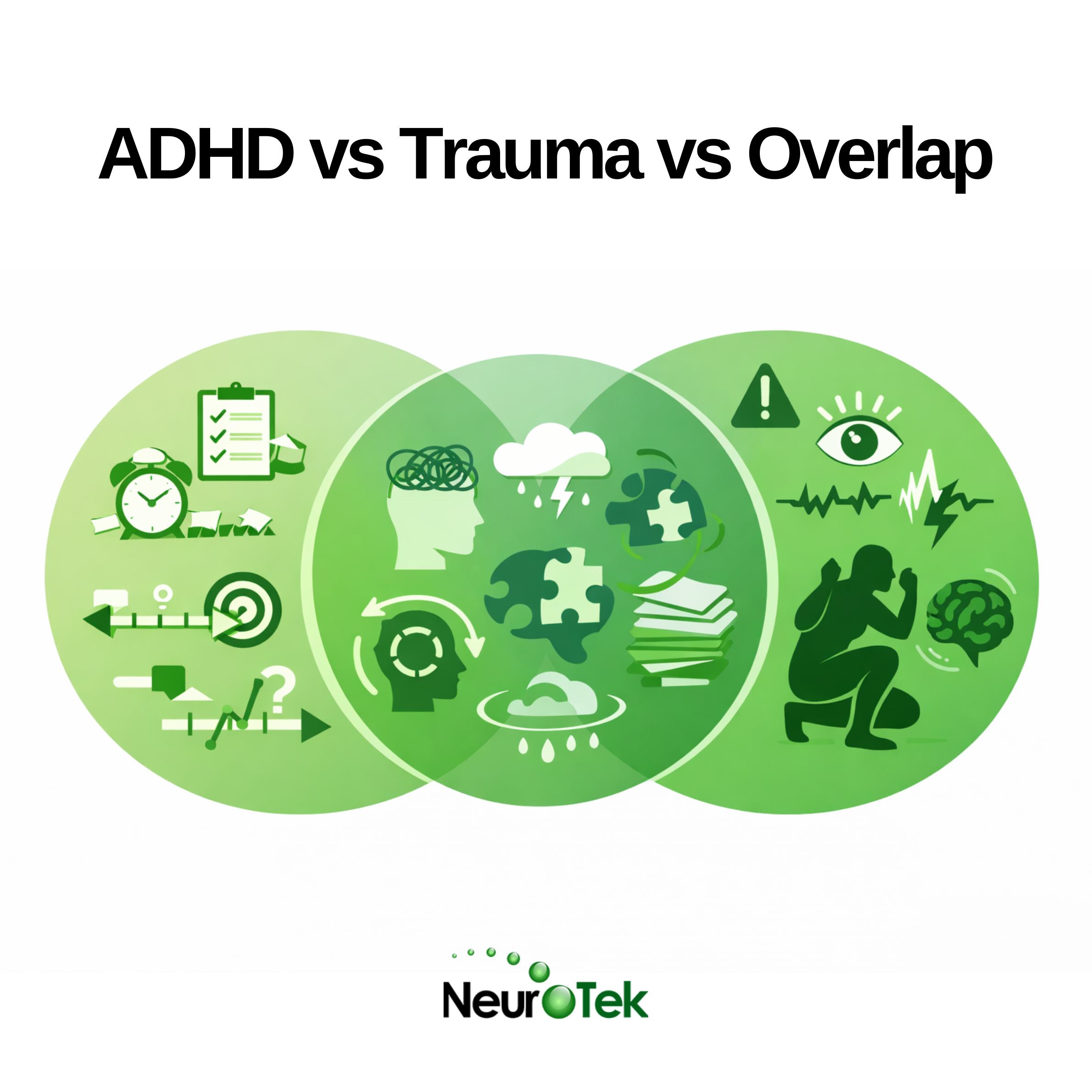
ADHD is not caused by trauma. However, trauma, chronic stress, and repeated failure experiences frequently co-occur with ADHD and can amplify symptoms.
Clear boundary:
ADHD ≠ trauma
ADHD + trauma = often more severe impairment
Establishing this distinction early matters for credibility — and for ethical treatment planning.
What EMDR Is Designed to Do
Eye Movement Desensitization and Reprocessing (EMDR) is a structured psychotherapy developed by Francine Shapiro to treat trauma and post-traumatic stress disorder (PTSD).
The Adaptive Information Processing (AIP) Model
EMDR is guided by the AIP model, which proposes that:
- The brain has a natural system for processing experiences
- Overwhelming events can become maladaptively stored
- These unprocessed memories continue to trigger emotional and physiological responses in the present
Through bilateral stimulation (eye movements, taps, or tones), EMDR helps the brain reprocess these memories so they lose their emotional charge.
What EMDR reliably treats
EMDR is recognized as an evidence-based treatment for PTSD by:
- World Health Organization
- American Psychiatric Association
- EMDR International Association
It is also used for trauma-related anxiety, phobias, and stress disorders.
What EMDR does not target directly
- Core attention regulation
- Baseline impulsivity
- Dopamine production
- Executive planning capacity
That distinction is non-negotiable.
Why EMDR Is Being Explored for ADHD
Despite not being an ADHD treatment, EMDR and ADHD are increasingly discussed together for several reasons.
Emotional dysregulation vs core ADHD symptoms
Many adults with ADHD experience emotional responses that are faster, stronger, and longer-lasting than expected. Trauma can intensify this pattern.
Rejection sensitivity and chronic shame
Repeated experiences of criticism, academic failure, bullying, or social rejection can create trauma-linked beliefs such as:
- “I’m broken”
- “I always mess things up”
- “I’m not good enough”
These beliefs fuel avoidance, procrastination, and emotional shutdown — often mistaken for “worsening ADHD.”
Developmental trauma overlays
So-called “small-t” traumas (chronic invalidation, inconsistent support) accumulate over time and may dysregulate the nervous system.
Stress-load amplification
Stress impairs the prefrontal cortex functioning in everyone. For ADHD brains, already operating with reduced executive bandwidth, trauma-related stress can dramatically magnify symptoms.
This is the gap EMDR aims to address.
Does EMDR Help ADHD Symptoms?
Short answer: Indirectly, sometimes.
What may improve
- Emotional reactivity
- Stress tolerance
- Trauma-linked avoidance
- Negative self-concept
- Shame-based procrastination
- Rejection sensitivity
What does not reliably improve
- Sustained attention
- Working memory capacity
- Baseline impulsivity
- Executive planning skills
- Time blindness
EMDR helps reduce emotional interference, not rewire ADHD neurology.
What the Research Actually Shows
The evidence base for EMDR for ADHD is emerging, not established.
What exists
- Case reports in children and adults
- Small pilot studies
- Systematic reviews examining EMDR in neurodevelopmental disorders
Notable findings include improvements in:
- Emotional regulation
- Trauma symptoms
- Executive functioning measures when trauma is present
What does not exist
- Large randomized controlled trials (RCTs)
- ADHD as a primary outcome variable
- Long-term comparative studies vs medication or CBT
Systematic reviews (e.g., Sopena et al., 2023) conclude EMDR may be feasible for neurodevelopmental populations but emphasize the need for stronger evidence.
Key limitation:
Most studies measure trauma outcomes — not ADHD core symptoms.
EMDR for ADHD With Trauma vs ADHD Alone
|
Profile |
Expected Outcome |
|
ADHD + trauma history |
Reduced emotional dysregulation, less shame, improved coping |
|
ADHD without trauma |
Limited benefit; core symptoms remain unchanged |
This distinction alone outperforms most competing articles.
EMDR Adaptations for ADHD Clients
Standard EMDR protocols may require modification for ADHD populations.
Why eye movements alone may fail
ADHD brains often seek stimulation; traditional bilateral eye movements may not sufficiently “tax” working memory.
Common adaptations
- Tactile bilateral stimulation (tappers)
- Auditory alternating tones
- Larger body movements
- Shorter processing sets
- Slower pacing and frequent grounding
Therapist experience matters more than the modality itself.
Risks, Limitations, and When EMDR Is Not a Fit
This section is often omitted — and that’s a red flag.
Potential risks
- Overstimulation
- Emotional flooding
- Dissociation in poorly screened clients
- False expectations of “curing ADHD”
EMDR may not be appropriate if:
- There is no trauma history
- The client is in acute crisis
- Executive supports are absent
- The therapist lacks ADHD-specific training
Transparency here builds trust — and backlinks.
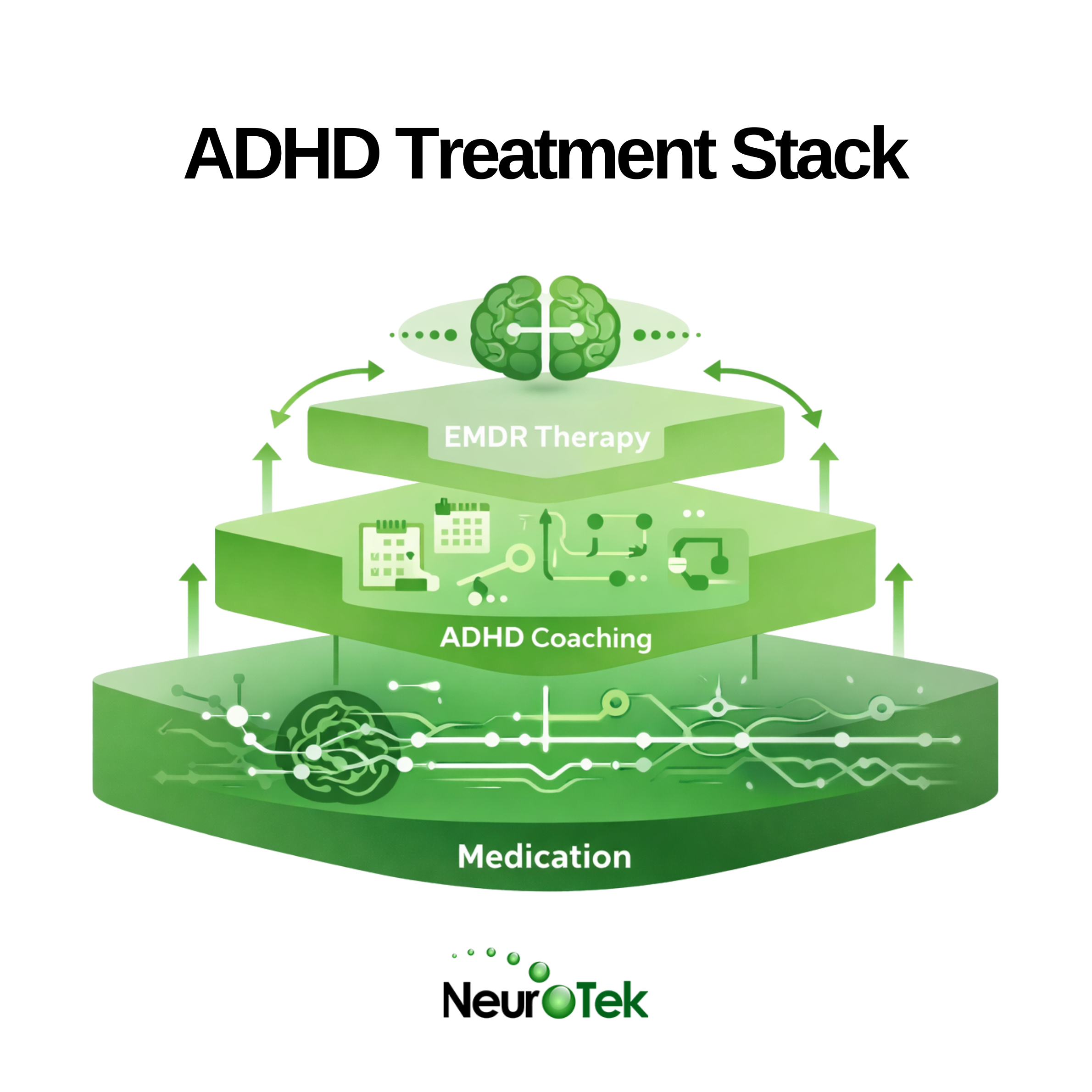
EMDR vs Other ADHD Interventions
|
Treatment |
Targets Core ADHD? |
Role |
|
Medication |
Yes |
First-line |
|
CBT |
Partially |
Skill development |
|
ADHD Coaching |
Yes |
Functional systems |
|
EMDR |
No |
Emotional burden reduction |
EMDR is best positioned as an adjunct, not a replacement.
Who Should Consider EMDR for ADHD
EMDR may be appropriate if:
- There is a history of trauma, bullying, or chronic invalidation
- Emotional dysregulation is disproportionate to ADHD severity
- Progress has plateaued with medication or coaching
- Shame and avoidance dominate daily functioning
Bottom Line — Is EMDR Good for ADHD?
Direct answer:
- EMDR is not a treatment for ADHD itself
- It can be valuable for trauma-related impairments that worsen ADHD
- It works best within a comprehensive treatment plan
That is the most accurate, defensible position available today.
Frequently Asked Questions
Can EMDR help with ADHD?
Yes — indirectly, when trauma or chronic stress significantly contributes to impairment.
Does EMDR improve focus?
Not reliably. Improved focus is usually secondary to reduced emotional overload.
Is there an EMDR ADHD protocol?
No standardized ADHD-specific protocol exists. Adaptations are clinician-driven.
Can EMDR replace medication?
No. EMDR does not address ADHD’s neurobiological core.
How long does EMDR take for ADHD-related issues?
From several sessions to months, depending on trauma complexity.
Sources
[1] National Institute of Mental Health — Attention-Deficit/Hyperactivity Disorder (ADHD)
https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd
[2] World Health Organization — Guidelines for the Management of Conditions Specifically Related to Stress
https://www.who.int/publications/i/item/WHO-MSD-MER-17.5
[3] American Psychological Association — Clinical Practice Guideline for the Treatment of PTSD
https://www.apa.org/ptsd-guideline/treatments/eye-movement-reprocessing
[4] Meentken, M. G., et al. (2017).
EMDR for PTSD in Children with ADHD and ASD.
European Journal of Psychotraumatology, 8(1).
https://pubmed.ncbi.nlm.nih.gov/28596979/
[5] de Jongh, A., et al. (2019).
EMDR Therapy for Complex PTSD and Comorbid Conditions.
European Journal of Psychotraumatology, 10(1).
https://pubmed.ncbi.nlm.nih.gov/31275677/
[6] Arnsten, A. F. T. (2009).
Stress Signalling Pathways That Impair Prefrontal Cortex Structure and Function.
Nature Reviews Neuroscience, 10(6), 410–422.
https://pubmed.ncbi.nlm.nih.gov/19455173/
[7] McEwen, B. S., & Morrison, J. H. (2013).
The Brain on Stress.
Nature Reviews Neuroscience, 14(8), 563–575.
https://pubmed.ncbi.nlm.nih.gov/23842499/