EMDR for Narcissistic Abuse
Jan 14th 2026
Survivors of narcissistic abuse don’t usually search for “trauma therapy” in general. They search for EMDR for narcissistic abuse specifically. That’s not an accident. Unlike a single-event trauma, narcissistic abuse is often characterized by 'death by a thousand cuts'—prolonged, repeated incidents that lead to Complex PTSD (C-PTSD). EMDR is uniquely equipped to untangle this web of interconnected memories
Most have already tried talk therapy, insight-oriented work, or CBT. They understand what happened. What hasn’t changed is how their body reacts, how shame shows up automatically, or why certain memories still feel emotionally present rather than past.
This guide explains why EMDR comes up so often in narcissistic abuse recovery, what it can realistically help with, and where its limits are. It will not promise quick fixes or “closure.” It will clarify when EMDR therapy for narcissistic abuse survivors is useful—and when it needs to be part of a broader, more integrated approach.
Why EMDR Comes Up in Narcissistic Abuse Recovery
Narcissistic abuse creates a specific kind of injury:
- Not just fear, but chronic self-doubt
- Not just sadness, but identity erosion
- Not just memories, but ongoing emotional reactivity
Survivors often describe feeling stuck in the past even after leaving the relationship. This happens because the nervous system still treats certain relational cues—tone of voice, criticism, withdrawal—as current threats.
EMDR for narcissistic abuse is frequently sought because it targets how traumatic memories are stored and activated, not just how they’re understood.
What this article will do:
- Explain what EMDR actually does well
- Clarify how narcissistic abuse differs from single-event trauma
- Set realistic expectations
What it will not do:
- Claim EMDR is a cure
- Oversimplify complex relational trauma
- Replace individualized clinical care
What People Mean by “Narcissistic Abuse” (and Why It’s Clinically Tricky)
“Narcissistic abuse” is not a formal DSM diagnosis. It’s a descriptive term used to capture a pattern of relational harm commonly associated with narcissistic traits.
Key dynamics include:
- Gaslighting (undermining reality perception)
- Chronic invalidation of emotions and needs
- Intermittent reinforcement (idealization → devaluation → withdrawal)
- Power asymmetry and control
Survivors frequently present with:
- Shame-based beliefs (“I’m defective,” “I caused this”)
- Identity confusion
- Complex trauma features without classic PTSD flashbacks
Critical clarification:
Abuse ≠ a formal diagnosis of Narcissistic Personality Disorder. Many people cause narcissistic harm without meeting full diagnostic criteria.
Clinically, this matters because treatment focuses on impact, not labels.
Why Narcissistic Abuse Is Different From “Single-Event” Trauma
Traditional PTSD models assume:
- A discrete traumatic event
- Clear before-and-after boundaries
Narcissistic abuse is different. It is typically:
- Repetitive
- Relational
- Subtle rather than overtly life-threatening
The effects cluster around:
- Self-concept: “I’m unlovable / invisible”
- Reality testing: “I can’t trust my perceptions”
- Attachment safety: “Closeness equals danger”
Clinical implication:
Trauma memories form clusters, not single targets. Treatment often requires sequencing, pacing, and extended preparation.
This is one reason standard protocols may need adaptation.

What EMDR Is Actually Designed to Do (Brief, Accurate Overview)
EMDR (Eye Movement Desensitization and Reprocessing) is a trauma-focused psychotherapy developed by Francine Shapiro.
It is grounded in the Adaptive Information Processing (AIP) model, which proposes that psychological distress arises when experiences are inadequately processed and stored in isolated memory networks.
What EMDR reliably does well:
- Reduces the emotional intensity of distressing memories
- Weakens trauma-linked negative beliefs
- Helps memories feel past rather than ongoing
What EMDR does not inherently do:
- Teach relational skills
- Build identity or boundaries
- Stop ongoing abuse
This distinction matters.
Does EMDR Help With Narcissistic Abuse?
Short answer: sometimes—under specific conditions.
Where EMDR May Help
EMDR therapy for narcissistic abuse survivors may be effective for:
- Repeated humiliation or degradation memories
- Betrayal and abandonment moments
- Boundary violations that still trigger shame or fear
It can reduce:
- Automatic self-blame
- Emotional flashbacks
- Nervous system overactivation
Many clients report that memories stop looping and begin to feel contextualized.
Where EMDR Is Often Insufficient Alone
EMDR does not rebuild:
- Identity
- Self-trust
- Relational discernment
It does not address:
- Ongoing manipulation
- Active contact with an abusive person
- Pattern recognition in relationships
Skills EMDR does not teach:
- Assertiveness
- Boundary-setting
- Reality testing
When EMDR May Be Premature
EMDR may not be appropriate early on if someone:
- Is still actively being abused
- Has significant dissociation without stabilization
- Lacks basic emotional regulation capacity
Preparation is not optional—it’s protective.
How EMDR Is Commonly Adapted for Narcissistic Abuse
Advanced clinicians increasingly recognize that narcissistic abuse represents atypical, pervasive trauma, often requiring protocol modifications—an approach reflected in continuing education endorsed by organizations like EMDR International Association.
Common adaptations include:
- Extended preparation and stabilization phases
- Emphasis on resource development
- Targeting core beliefs (“I don’t matter,” “I deserved this”)
- Working with relational patterns rather than isolated events
EMDR is often combined with:
- Parts-based approaches
- Psychoeducation
- Boundary and safety work
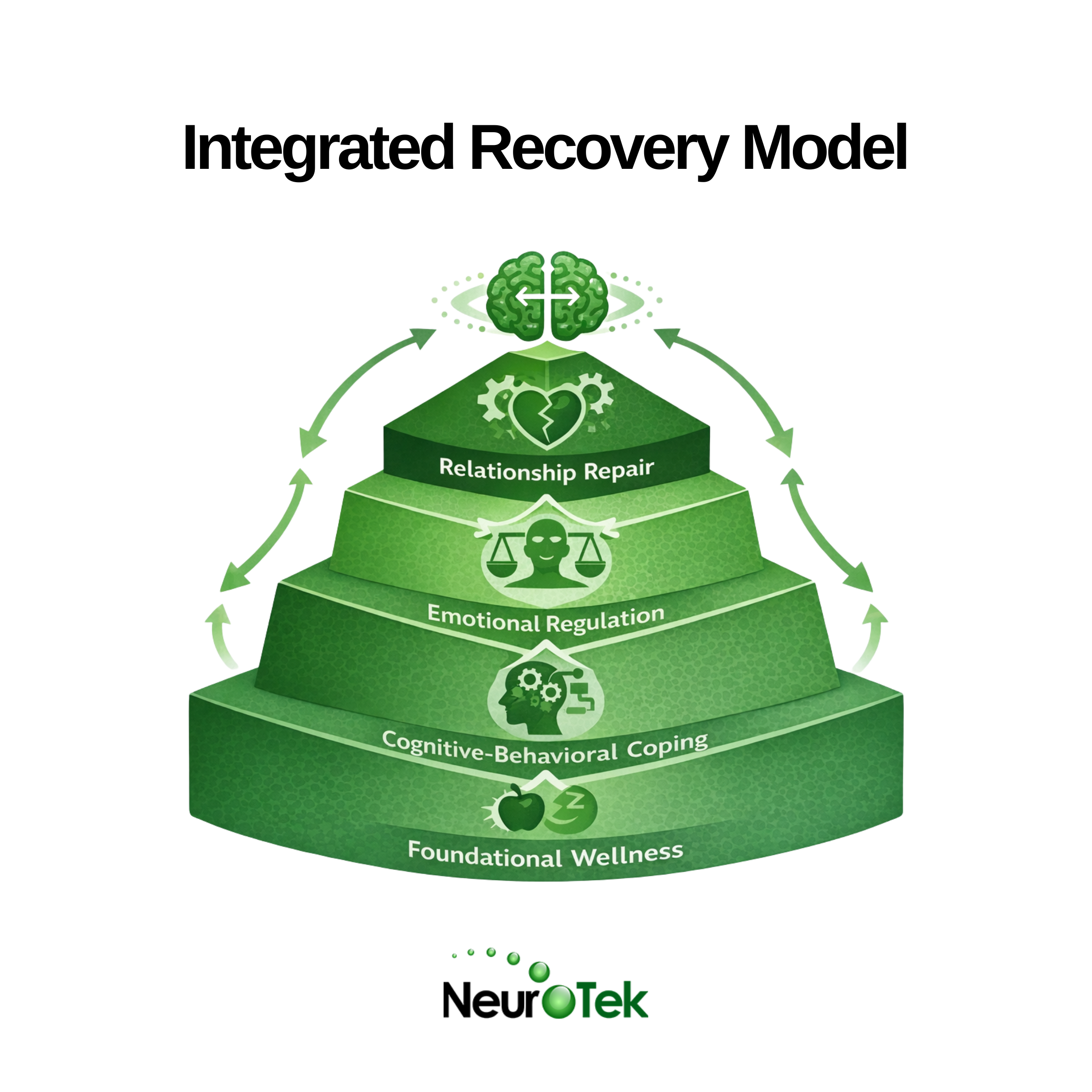
This integrated approach aligns better with how relational trauma actually presents.
What the Research Actually Says (and Doesn’t Say)
There are no large-scale randomized controlled trials specifically on EMDR for narcissistic abuse.
What exists:
- Strong evidence for EMDR in PTSD and complex trauma
- Clinical case reports and practitioner consensus
- Meta-analyses showing large effect sizes for trauma-related symptoms (e.g., Hedges’ g ≈ 1.2–1.3 in interpersonal trauma contexts)
Translation:
EMDR is not a proven cure for narcissistic abuse. It is a well-supported tool when used within a broader, trauma-informed treatment plan.
EMDR vs Other Approaches for Narcissistic Abuse Recovery
High-functioning recovery is rarely single-modality.
- EMDR → Memory reprocessing
- IFS / parts work → Identity repair, internal safety
- Schema therapy → Long-standing relational patterns
- Somatic approaches → Nervous system regulation
The most effective care positions EMDR as complementary, not dominant.
What Survivors Should Consider Before Starting EMDR
Questions to ask a therapist:
- Experience with complex relational trauma?
- Will EMDR be integrated with other modalities?
- How is preparation handled?
Red flags:
- Promising “closure”
- Skipping stabilization
- Rushing memory processing
Green flags:
- Willingness to go slow
- Emphasis on safety and pacing
- Clear boundaries and informed consent
Where Neurotek Fits
Neurotek tools can support regulation and bilateral stimulation as adjuncts, not replacements, for therapy.
Important clarifications:
- Devices ≠ therapy
- Best used alongside professional guidance
- Most effective when integrated into a clinician-led plan
Technology supports healing—it does not substitute for it.
Bottom Line: A Clear, Honest Conclusion
EMDR for narcissistic abuse can help process traumatic memories, reduce shame, and calm nervous system reactivity.
It does not:
- Repair identity on its own
- Teach boundaries
- Replace relational healing
Survivors benefit most from:
- Integrated, trauma-informed care
- Realistic expectations
- Clinicians who understand relational abuse dynamics
If this guide was helpful, consider sharing it or exploring Neurotek’s related educational resources.
Sources
[1] EMDR International Association — What Is EMDR Therapy?
https://www.emdria.org/about-emdr-therapy/
[2] American Psychological Association — Clinical Practice Guideline for the Treatment of PTSD
https://www.apa.org/ptsd-guideline/treatments/eye-movement-reprocessing
[3] World Health Organization — Guidelines for the Management of Conditions Specifically Related to Stress
https://www.who.int/publications/i/item/WHO-MSD-MER-17.5
[4] National Institute for Health and Care Excellence — PTSD Guideline (NG116)
https://www.nice.org.uk/guidance/ng116
[5] Cloitre, M., et al. (2012).
A Developmental Approach to Complex PTSD: Childhood and Adult Cumulative Trauma as Predictors of Symptom Complexity.
Journal of Traumatic Stress, 25(4), 399–408.
https://pubmed.ncbi.nlm.nih.gov/22806741/
[6] de Jongh, A., et al. (2019).
Complex PTSD and EMDR: A Review of Evidence and Clinical Practice.
European Journal of Psychotraumatology, 10(1).
https://pubmed.ncbi.nlm.nih.gov/31275677/