EMDR for Addiction
Dec 12th 2025
Addiction is rarely just about substances or behaviors. It’s tightly intertwined with memory, learning, survival responses, conditioning, and emotional regulation. That’s why EMDR for addiction has become a topic of interest across treatment centers, researchers, and clinicians.
People exploring EMDR therapy for addiction want clarity about one key question:
Can EMDR help with addiction by targeting the psychological drivers—trauma, triggers, cravings, and compulsive cycles—that influence substance use and behavioral addictions?
Here’s the grounded truth:
- EMDR is not a substitute for medical detox, rehab, or medication-assisted treatment.
- It is a trauma-focused psychotherapy used within comprehensive addiction treatment plans.
- Its role depends on whether addiction is trauma-linked, habit-driven, reward-conditioned, or emotionally reinforced.
This guide merges the strongest insights from clinical literature, addiction research, and EMDR practice—giving you a high-authority overview without overstating what EMDR can do.
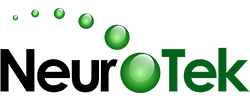
What “Addictive Memory Networks” Actually Are
Addiction is not just chemical dependence—it’s learning. The brain forms high-intensity memory networks that link:
- emotional relief
- sensory cues
- context
- compulsive behavior
- anticipated reward
These “addictive memory networks” can become hyper-reactive, meaning:
- A smell
- A place
- A feeling
- A conflict
- A bodily sensation
…can trigger cravings or compulsive responses before conscious thought even begins.
Trauma-Linked Addiction
Some people use substances or behaviors (alcohol, opioids, gambling, sex, porn, food) to regulate overwhelming emotional states tied to unresolved trauma.
Habit-Driven Addiction
Others develop addiction through repetition, reinforcement, and routine—not necessarily trauma.
Reward-Sensitive Addiction
In some cases, the brain becomes highly sensitized to dopamine-driven reward pathways.
Where EMDR Relates
EMDR therapy for addiction treatment is sometimes used to target:
- emotionally charged memories
- trauma-linked triggers
- shame-based schemas
- compulsive loops tied to specific feelings
- internal cues that activate cravings
But not every addiction is trauma-based. Competitors often hide this nuance.
How EMDR Is Used in Addiction Treatment Settings
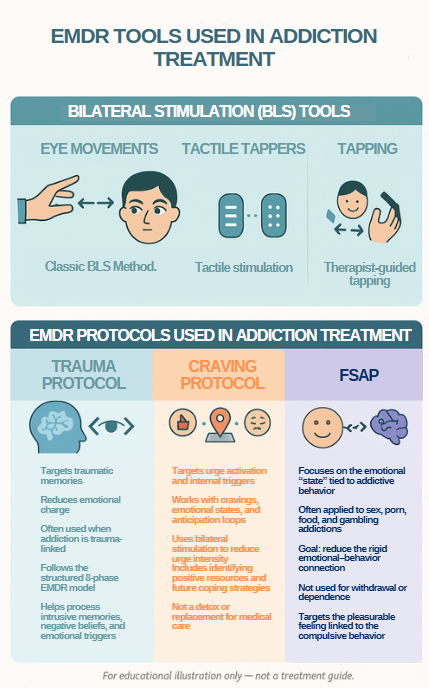
EMDR (Eye Movement Desensitization and Reprocessing) uses dual-attention bilateral stimulation—usually eye movements, taps, tones, or pulsers—to help clients process emotionally intense memories within a structured protocol.
Clinically, EMDR is applied in two broad ways:
EMDR for Trauma
The traditional model targets:
- intrusive memories
- negative self-beliefs
- emotional dysregulation
- trauma reminders
- hyperarousal
This can indirectly influence addiction patterns when the addiction developed as a coping strategy.
EMDR Adapted for Addiction Cravings or Triggers
Some EMDR clinicians use addiction-focused protocols designed to:
- reduce urge intensity
- decrease cue-reactivity
- target body-based craving sensations
- disrupt emotion–behavior linkages
EMDR is never used as a standalone detox solution.
It is one component within a larger clinical plan.
Theoretical Mechanisms: How EMDR May Influence Addiction-Related Patterns
Research is ongoing, but four theoretical pathways help explain why EMDR is used in addiction settings.
Reducing the Emotional Intensity of Trauma-Linked Triggers
Many addictions are attempts to regulate:
- fear
- shame
- grief
- loneliness
- helplessness
EMDR sometimes helps reprocess the memories or sensations associated with these states, reducing the emotional charge that previously drove coping behaviors.
Working Memory Taxation and Craving Reduction
Eye movements compete with internal mental imagery for working memory capacity.
Some studies suggest this may:
- reduce the vividness of craving imagery
- weaken the emotional pull of urges
- help interrupt compulsive loops
This is relevant across both:
- substance addictions
- behavioral addictions (sex, porn, gambling, food)
Expectancy Violation
Addictive patterns often rely on rigid predictions:
“If X happens, I have to use.”
EMDR’s dual-attention process may help interrupt these automatic emotional predictions—creating space for new coping strategies.
Cue-Reactivity and Deconditioning
Addiction isn’t just about external cues.
Internal cues—sensations, emotions, memories—are often the real drivers.
Some EMDR protocols focus specifically on internal cue-reactivity.
EMDR Protocols Used in Addiction Treatment
Standard EMDR 8-Phase Protocol
A safe, compliance-friendly overview:
- History taking
- Preparation
- Assessment
- Desensitization
- Installation
- Body scan
- Closure
- Reevaluation
These target emotionally charged memories—not the addiction itself.
Addiction-Specific EMDR Approaches
DeTUR (Desensitization of Triggers & Urge Reprocessing)
Used to address:
- urge activation
- craving intensity
- emotional states preceding use
FSAP (Feeling-State Addiction Protocol)
Often used for:
- sex addiction
- porn addiction
- food addiction
- compulsive shopping
FSAP focuses on the “positive feeling state” linked to compulsive behavior.
Craving-Focused EMDR
Targets:
- craving imagery
- somatic sensations
- reinforcing emotional loops
EMDR Integrated With Relapse-Prevention Models
Clinicians may combine:
- EMDR
- CBT relapse-prevention
- skills training
- motivational approaches
Integration is the trend—not EMDR alone.
EMDR for Different Types of Addiction
Substance Use Disorders
Alcohol, opioids, stimulants, cannabis, GHB, nicotine, etc.
Many clients have comorbid trauma (PTSD, childhood adversity, combat exposure). EMDR is sometimes used to target those trauma symptoms.
Behavioral Addictions
EMDR for Sex Addiction
FSAP is often referenced.
Focuses on:
- shame cycles
- intrusive imagery
- emotional triggers
EMDR for Porn Addiction
Addresses:
- compulsive loops
- cue-sensitivity
- emotional avoidance patterns
EMDR for Food Addiction
Targets:
- emotional eating
- body-based sensations
- shame-driven patterns
When Addiction Is Not Trauma Driven
Important clinical nuance:
- EMDR cannot resolve neurochemical dependence.
- EMDR is not a detox method.
- EMDR is applied when trauma or emotional learning contributes to addictive cycles.
What the Research Says
A medically compliant summary:
EMDR + PTSD + Substance Use Comorbidity
Research consistently supports EMDR for PTSD.
When PTSD decreases, some addiction-related symptoms may shift as well—though this is a secondary observation, not a direct causal claim.
EMDR and Craving Research
Some small studies suggest:
- reduced craving intensity
- reduced cue reactivity
- reduced emotional arousal
These findings are early and require more research.
What Has NOT Been Proven
- No definitive evidence that EMDR treats addiction itself
- No guarantee of relapse-prevention
- No replacement for medication or detox
- No universal results
What to Expect in an EMDR Session for Addiction
Clinically realistic expectations:
- You review history and emotional triggers
- You learn stabilization strategies
- You identify target memories or internal cues
- You proceed only if stable and prepared
- Sessions may evoke strong emotions (normal)
- Addiction-focused EMDR moves more slowly than trauma-only work
Therapists prioritize safety, pacing, and stabilization.
When EMDR May Not Be a Fit
- Active withdrawal
- Severe dissociation
- Unmanaged bipolar or psychosis symptoms
- Medical instability
- Addiction unrelated to emotional learning
- Inability to tolerate memory work
- When the primary need is immediate detox or medical stabilization
Choosing an EMDR Therapist for Addiction Work
Clinically competent providers typically have:
- EMDRIA-approved training
- Experience with addiction populations
- Familiarity with DeTUR, FSAP, and craving protocols
- A stabilization-first approach
- Clear boundaries and safety planning
Red flags:
- Anyone promising EMDR will “cure addiction”
- Anyone skipping preparation phases
- Anyone offering EMDR without addiction training
What People Usually Ask Before Starting EMDR for Addiction
Not promises—clarifications.
“Does EMDR help with addiction?”
It may help address the emotional and trauma-related factors linked to some addictions.
“What if my addiction isn’t trauma-related?”
EMDR may still be used for craving or urge work, depending on the clinician.
“Can EMDR make cravings worse?”
Some people report temporary emotional shifts; clinicians plan for this.
“What if I don’t remember a trauma?”
EMDR can target sensations, emotions, or present-day triggers—not just memory.
“Will EMDR be overwhelming?”
Therapists use stabilization first to keep sessions within tolerance.
FAQs (Short, Safe & Search-Optimized)
Does EMDR help with addiction?
It may support trauma-related symptoms and triggers that influence addictive behavior.
Can EMDR reduce cravings?
Some early research suggests reductions in craving intensity in certain cases.
Is EMDR used for sex or porn addiction?
Yes—protocols like FSAP are sometimes applied.
Is EMDR effective without trauma?
It depends on the role emotional learning plays in the addiction.
Is EMDR part of addiction treatment programs?
Many programs integrate EMDR with other therapeutic approaches.
Final Takeaway
EMDR is not a detox tool, a standalone addiction treatment, or a guaranteed relapse-prevention method.
But when addiction is tied to trauma, emotional learning, or internal triggers, EMDR addiction therapy can play a meaningful role within a broader, individualized treatment plan.
Its strongest evidence lies in trauma-focused outcomes—with emerging, but not definitive, findings on craving, compulsive behavior, and urge reduction. Anyone considering EMDR should work with a clinician trained in both trauma and addiction dynamics.
Sources
[1] EMDR Institute, Inc. — What Is EMDR Therapy?
https://www.emdr.com/what-is-emdr/
[2] American Psychological Association (APA) — Clinical Practice Guideline for the Treatment of PTSD
https://www.apa.org/ptsd-guideline/treatments/eye-movement-reprocessing
[3] National Center for PTSD (VA/DoD 2023) — PTSD Clinical Practice Guidelines
https://www.ptsd.va.gov/professional/treat/treatessentials/cpg_ptsd_management.asp
[4] World Health Organization (WHO) — Post-Traumatic Stress Disorder
https://www.who.int/news-room/fact-sheets/detail/post-traumatic-stress-disorder
[5] National Institute for Health and Care Excellence (NICE UK) — PTSD Guidelines
https://www.nice.org.uk/guidance/ng116
PMC Article: Post-traumatic stress disorder in primary care
https://pmc.ncbi.nlm.nih.gov/articles/PMC6592320/
[6] PubMed — Efficacy of EMDR for PTSD: Meta-analysis of Randomized Controlled Trials
https://pubmed.ncbi.nlm.nih.gov/25101684/
[8] Hase, M., Schallmayer, S., & Sack, M. (2008) — EMDR vs. CBT in the Treatment of PTSD
https://pubmed.ncbi.nlm.nih.gov/18799356/
[9] Markus, W., et al. (2017) — EMDR Effects on Craving and Addiction-Related Symptoms (Literature Review)
https://pubmed.ncbi.nlm.nih.gov/28504081/
[10] National Institute on Drug Abuse (NIDA) — The Science of Drug Use & Addiction
https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction
[11] CDC — Adverse Childhood Experiences (ACE Study) and Addiction Risk
https://www.cdc.gov/violenceprevention/aces/index.html
[12] PubMed Central — EMDR Therapy for Anxiety and Panic Symptoms
https://pmc.ncbi.nlm.nih.gov/articles/PMC3951033/
[13] Springer — EMDR in Addictions: Mechanisms, Evidence & Protocol Adaptations
https://link.springer.com/article/10.1007/s10615-020-00758-4
[14] National Library of Medicine — Childhood Trauma as a Predictor of Substance Dependence
https://pubmed.ncbi.nlm.nih.gov/26077722/
[15] PubMed — Working Memory Taxation & Craving Reduction Mechanisms
https://pubmed.ncbi.nlm.nih.gov/25705912/