EMDR For OCD
Dec 12th 2025
Interest in EMDR for OCD has surged in recent years, especially among people who feel stuck after trying standard treatments like Exposure and Response Prevention (ERP) or cognitive behavioral therapy (CBT). Some seek EMDR therapy for OCD because their symptoms feel emotionally charged or linked to past experiences. Others turn to EMDR because talk therapy hasn’t reduced the intensity of their intrusive thoughts.
But here’s the truth clinicians rarely say directly:
OCD is not a trauma disorder, and EMDR was not originally designed for OCD.
The research is promising in some areas, inconclusive in others, and still evolving overall.
This guide does not promise outcomes. It clarifies the landscape so you can make informed decisions based on evidence, not hype.
Understanding OCD: Why Intrusive Thoughts Aren’t “Random”
What OCD Actually Is — Beyond Stereotypes
OCD is far more complex than the pop-culture caricature of handwashing or organizing. It involves:
Obsessions
Intrusive, unwanted experiences that may appear as:
- Thoughts (“What if I poison someone?”)
- Images (violent or disturbing mental pictures)
- Sensations (a feeling of contamination or “wrongness”)
- Urges (“Push the steering wheel and crash the car”)
These are not voluntary and not reflective of intent. They trigger distress because they violate the person’s values.
Compulsions
Compulsions can be:
- Overt behaviors: washing, checking, tapping, arranging
- Mental rituals: analyzing, reviewing memories, praying, counting
- Avoidance: staying away from triggers, withdrawing from situations
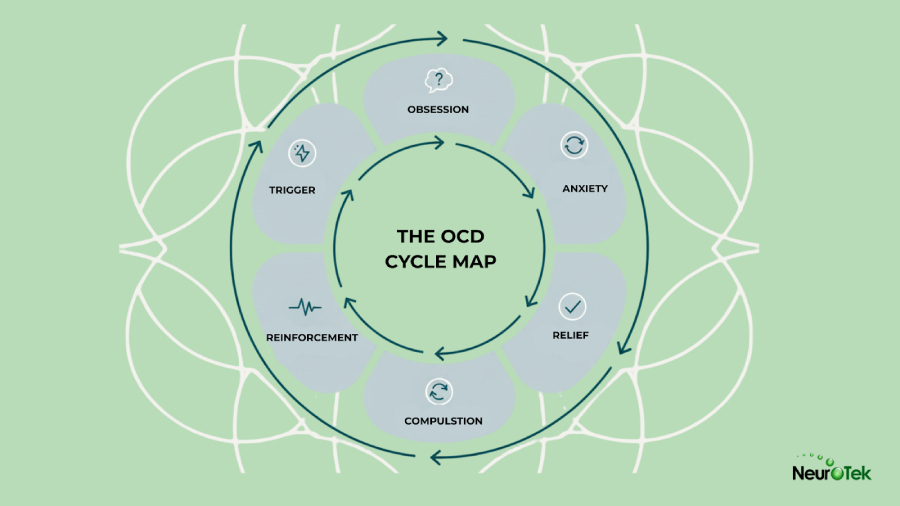
The compulsion temporarily reduces anxiety — which reinforces the OCD cycle.
The Core Mechanisms
OCD is driven by:
- Intolerance of uncertainty
- Catastrophic misinterpretations (“If I thought it, it must mean something”)
- Overactive threat detection systems
- Distress intolerance
This matters because EMDR targets emotional activation, not the cognitive distortions or behavioral loops that maintain OCD.
OCD Subtypes That Intersect With EMDR-Related Questions
Certain OCD presentations feel emotionally charged, shame-based, or tied to past experiences — making people wonder whether EMDR therapy for OCD could help.
Harm OCD
Intrusive fears of causing harm, often accompanied by overwhelming shame and alarm.
Contamination OCD
Not just fear of germs — often disgust-based or tied to symbolic meanings.
Sexual or Religious Intrusive Thoughts
Highly distressing, often associated with guilt, fear of moral failure, or shame.
“Just Right” or Sensory OCD
Driven not by fear of danger, but by an intolerable internal sensation of incompleteness.
Relationship OCD
Obsessions about whether one’s feelings or relationship is “correct.”
Existential OCD
Intrusive questions about reality, meaning, or one’s identity.
Some of these themes overlap with trauma-like emotional responses (shame, disgust, panic).
Others don’t resemble trauma processing at all.
This difference is central to understanding when EMDR makes sense.
OCD, Stress, and Memory
Stress doesn’t cause OCD, but it can intensify activation in:
- threat circuits
- emotional memory networks
- catastrophic interpretation pathways
Many people with OCD report moments where past experiences feel linked to present obsessions — even if not traumatic.
Examples:
- A person bullied for “being dirty” develops contamination themes.
- A strict religious upbringing contributes to scrupulosity.
- Past relational instability fuels relationship OCD.
These are meaning-based associations, not trauma in the clinical sense.
But they can increase emotional activation — which is where EMDR may offer benefit.
What EMDR Actually Is (Stripped of the Hype)
Core Components
EMDR (Eye Movement Desensitization and Reprocessing) uses:
- bilateral stimulation (eye movements, tapping, or tones)
- memory recall
- structured protocols
- AIP model (Adaptive Information Processing)
The goal:
Help the brain integrate distressing memories or emotional material that feels “stuck.”
The standard EMDR process includes eight phases, focusing on history taking, preparation, assessment, desensitization, installation, body scan, closure, and reevaluation.
What EMDR Tries to Do — Theoretically, Not Medically
EMDR is thought to:
- reduce emotional charge linked to distressing memories
- activate natural memory reconsolidation processes
- help clients reprocess unintegrated emotional experiences
- reduce physiological reactivity
This works well for PTSD because PTSD is a disorder based on unprocessed traumatic memories.
OCD is not.
Why Some Clinicians Adapt EMDR for OCD
Clinicians sometimes modify EMDR for OCD when:
- intrusive thoughts feel emotionally overwhelming
- shame, disgust, or panic intensify symptoms
- traumatic events appear connected to themes
- clients cannot tolerate ERP without emotional regulation help
- the OCD onset occurred after trauma
Adaptations might target:
- the first time the obsession appeared
the worst episode of symptom-related distress - memories linked to shame or fear
- emotional triggers
- the distress provoked by the obsession itself
Some clinicians use EMDR during exposure-like imagery to reduce activation, though this is not standard.
What Research Suggests — And Why It’s Not Conclusive
Here’s the honest landscape — without overclaiming.
What Current Research Looks Like
Most EMDR/OCD studies involve:
- small participant groups
- varying EMDR protocols
- mixed methodologies
- inconsistent follow-up periods
- different OCD severities
- some combining EMDR with ERP
This means results cannot be generalized.
Key Areas Researchers Have Explored
Studies have investigated:
- reductions in distress linked to obsessions
- shifts in emotional intensity
- decreases in compulsive urges
- improvements in comorbid anxiety or depression
- EMDR as an alternative when ERP fails
- EMDR as an additional tool for trauma-linked OCD
- EMDR + ERP combinations
Some findings suggest EMDR may be comparable to CBT for certain patients.
Others show EMDR helps when ERP alone is intolerable.
But the research is early — promising, not definitive.
Why Evidence Isn’t Uniform
OCD is not one condition.
Different subtypes respond differently.
Key variables include:
- presence of trauma
- insight level
- emotional reactivity
- type of obsession
- whether compulsions are behavioral or mental
- whether the obsession has memory-based content
There is no standardized EMDR protocol for OCD, which complicates conclusions.
How EMDR Is Used for OCD in Clinical Practice
1. Approaches Therapists May Use
Processing past emotionally significant events
Not because trauma caused OCD, but because emotional processing can reduce reactivity.
Targeting emotional distress around specific obsessions
For example, the shame linked to sexual intrusive thoughts.
Working directly with present triggers
Imagery of feared scenarios while using bilateral stimulation.
Using EMDR during exposure-like exercises
Some clinicians integrate EMDR with ERP principles.
The Distancing Approach
Developed to help clients separate themselves from intrusive thoughts, reducing fusion and reactivity.
Resource building and emotional regulation
Strengthening grounding skills before exposure work.
What EMDR Doesn’t Do
Let’s be blunt:
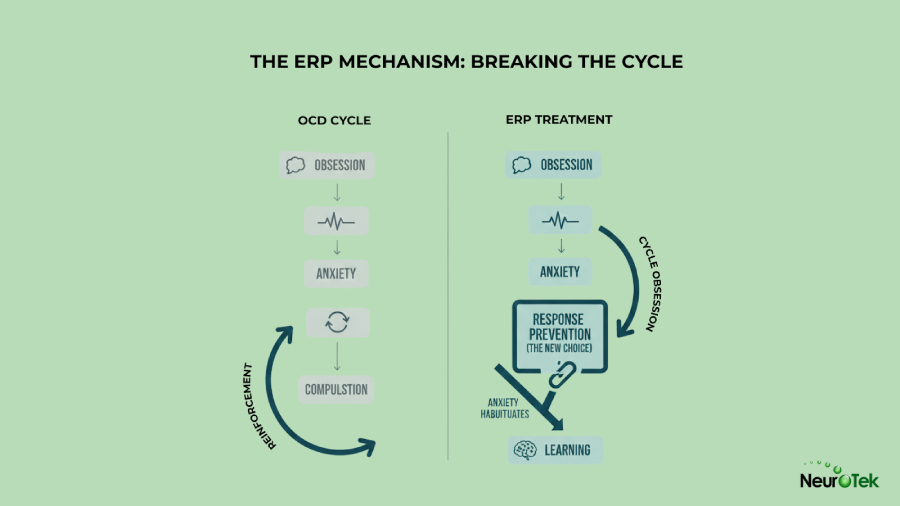
- EMDR does NOT replace ERP.
- It does NOT erase intrusive thoughts.
- It does NOT remove compulsions by itself.
- It does NOT guarantee symptom change.
ERP remains the gold-standard treatment for OCD.
EMDR may support ERP — it does not replace it.
The Realistic, Grounded Frame
Outcomes vary:
- Some people experience meaningful improvement.
- Some notice reduced emotional charge around triggers.
- Some feel no significant benefit.
- Some experience temporary symptom spikes before settling.
There is no universal response profile.
Potential Risks, Limitations & Situations Where EMDR May Not Fit
People need to hear this clearly — EMDR is not low-risk for every OCD presentation.
1. Emotional flooding
Bilateral stimulation can increase activation if pacing is too fast.
2. Temporary symptom spikes
Increased access to intrusive thoughts can worsen distress temporarily.
3. Heightened awareness of internal experiences
This can exacerbate rumination or checking.
4. Poor insight complicates treatment
When clients believe obsessions reflect actual danger, EMDR may increase uncertainty.
5. Trauma work may derail OCD treatment structure
Some clients shift focus away from compulsions, delaying progress.
6. Bilateral stimulation may intensify looping
Some clients experience increased cognitive cycling.
7. Not all OCD subtypes align with EMDR mechanisms
Especially those without memory-linked content.
Why People Start to Explore EMDR for OCD
Clients often consider EMDR therapy when:
- ERP feels too overwhelming
- trauma appears intertwined with symptoms
- shame or disgust drives the obsessions
- emotional reactivity is high
- compulsions aren’t the main issue
- they plateaued in CBT
- they want more than cognitive reframing
EMDR can function as an emotional regulation tool or as a bridge to ERP.
EMDR vs. ERP vs. CBT
Here’s the clearest breakdown you’ll find online.
EMDR
Focus:
- emotional integration
- memory networks
- reducing physiological activation
Strengths:
- lowers emotional reactivity
- helpful for trauma-linked OCD
- useful for shame-based or panic-based themes
Limitations:
- doesn’t break compulsions
- doesn’t build uncertainty tolerance
ERP
Focus:
- behavioral change
- resisting compulsions
- increasing uncertainty tolerance
Strengths:
- strongest evidence
- works across OCD subtypes
Limitations:
- emotionally challenging
- high dropout rates
CBT
Focus:
- distorted beliefs
- catastrophic interpretation
- cognitive restructuring
Strengths:
- pairs well with ERP
- improves insight
Limitations:
- not enough on its own for many patients
Combined Approaches
Clinicians may:
- use EMDR to reduce emotional distress
- follow with ERP to break compulsions
- integrate CBT to challenge misinterpretations
This tri-layer approach is increasingly common.
What People Usually Want to Know Before Starting EMDR
1. Does EMDR work for OCD?
It may help reduce distress for some people, especially when trauma or strong emotional activation is involved.
It is not a guaranteed or standalone treatment.
2. Can EMDR make OCD worse?
Yes — temporary worsening can occur.
Especially with poor insight, high rumination, or certain subtypes.
3. How long does EMDR take for OCD themes?
Highly variable. There is no standard timeline.
4. Is EMDR helpful for intrusive thoughts?
It can reduce emotional distress but doesn’t prevent intrusive thoughts from appearing.
5. Should I try EMDR before or after ERP?
Most clinicians recommend ERP first or using EMDR as an adjunct.
6. Is EMDR useful if I don’t have trauma?
Sometimes — but less predictable.
7. How do therapists decide what to target?
They evaluate:
- onset events
- emotional triggers
- meanings linked to obsessions
- avoidance patterns
- past experiences that amplify distress
Questions to Ask an EMDR Therapist About OCD
- Do you have experience adapting EMDR for OCD?
How do you decide what memories or triggers to process? - How do you prevent emotional flooding?
- Do you integrate ERP principles?
- How do you handle symptom spikes?
- How do you measure progress for OCD specifically?
These questions separate trained clinicians from generalists.
Frequently Asked Questions
Is EMDR good for OCD?
It can be helpful for some people, especially when emotional or trauma-related factors are significant.
Does EMDR work on compulsions?
Not directly. ERP remains essential.
What EMDR protocol is used for OCD?
There is no universal protocol; clinicians adapt EMDR based on the AIP model.
Can EMDR replace ERP?
No. EMDR may support ERP but cannot replace it.
Does EMDR help harm OCD?
Sometimes — especially when shame, guilt, or panic fuel the obsession.
Will EMDR stop intrusive thoughts?
No therapy can stop intrusive thoughts entirely.
Does bilateral stimulation calm OCD triggers?
It may reduce emotional arousal but is not a cure.
Conclusion
OCD is complex, and recovery requires evidence-based strategies.
EMDR for OCD can be useful:
- when trauma overlaps with symptoms
- when emotional activation is high
- when ERP alone is intolerable
- when shame or disgust drives the obsession
But EMDR is not a cure, not a replacement for ERP, and not universally effective.
When used appropriately and integrated into a broader treatment plan, EMDR can support meaningful progress — not by removing OCD, but by helping people engage more effectively in the treatments that do.
Sources
[1] National Institute of Mental Health — Obsessive-Compulsive Disorder (OCD)
https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd
[2] Abramowitz, J. S., Taylor, S., & McKay, D. (2009).
Obsessive-Compulsive Disorder.
The Lancet, 374(9688), 491–499.
https://pubmed.ncbi.nlm.nih.gov/19665647/
[3] Rachman, S. (1997).
A Cognitive Theory of Obsessions.
Behaviour Research and Therapy, 35(9), 793–802.
https://pubmed.ncbi.nlm.nih.gov/9299799/
[4] National Institute for Health and Care Excellence — OCD and Body Dysmorphic Disorder: Treatment (CG31)
https://www.nice.org.uk/guidance/cg31
[5] Foa, E. B., et al. (2005).
Randomized, Placebo-Controlled Trial of Exposure and Ritual Prevention for OCD.
American Journal of Psychiatry, 162(1), 151–161.
https://pubmed.ncbi.nlm.nih.gov/15625214/
[5] EMDR International Association — What Is EMDR Therapy?
https://www.emdria.org/about-emdr-therapy/
[6] Nazari, H., et al. (2011).
Comparison of EMDR and CBT in the Treatment of OCD.
Journal of Anxiety Disorders, 25(1), 1–8.
https://pubmed.ncbi.nlm.nih.gov/21095131/
[7] Böhm, K., et al. (2020).
Trauma-Focused Interventions in OCD With Comorbid PTSD.
European Journal of Psychotraumatology, 11(1).
https://pubmed.ncbi.nlm.nih.gov/32774765/