EMDR for Depression
Dec 11th 2025
Depression isn’t one problem—it’s a spectrum of conditions shaped by biology, history, stress exposure, and the way the brain stores experience. This is exactly why one-size-fits-all treatments often fall short. Medication helps some people dramatically; others experience little change. Traditional talk therapy works for many but doesn’t always touch the deeper roots of persistent negative beliefs or unresolved memories.
EMDR therapy for depression is gaining attention because it targets a dimension most treatments barely address: the memory networks that shape mood, self-worth, and emotional reactions long after the original event has passed.
For people whose depressive symptoms are tied to past adversity, EMDR can be a powerful non-pharmacological treatment—one that shifts the underlying emotional architecture rather than simply improving symptoms at the surface level.
This guide breaks down the science, the mechanisms, the research, the limitations, and the practical realities of using EMDR for depression.
Why EMDR Is Being Explored for Depression
Depression Isn’t Always a “Mood Disorder” in the Way People Think
Depression is often described as a chemical imbalance or a mood problem. That’s simplistic. For many people, depressive symptoms are shaped by:
Stored adverse memories
Events that were never fully processed—childhood criticism, emotional neglect, humiliations, failures, losses—can remain “stuck” in the nervous system.
Learned emotional patterns
The brain forms patterns based on past experience. If helplessness or worthlessness were learned early, they may surface automatically.
Negative self-beliefs formed after stressful events
Beck’s cognitive theory (1979) describes depression as rooted in beliefs about self, world, and future. EMDR directly targets where those beliefs formed.
Why Trauma-Linked Depression Responds Differently
Not all depression is trauma-based, but a large portion is shaped by unresolved life events—including “small-t trauma” (chronic stress, criticism, emotional invalidation). These experiences often create core beliefs like:
- “I’m not good enough.”
- “I’m defective.”
- “Nothing will ever get better.”
Traditional talk therapy strengthens coping.
Medication supports neurotransmitter regulation.
But neither directly rewires the memory networks that created these beliefs in the first place.
EMDR does.
How EMDR Therapy Approaches Depression
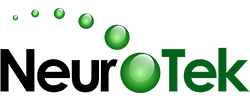
The Adaptive Information Processing (AIP) Model
AIP is the backbone of EMDR. It proposes:
- The brain naturally processes experiences and stores them adaptively.
- Trauma or highly stressful events can become stuck in a raw, state-specific form.
- These unprocessed memories continue to influence current thoughts, body sensations, and mood.
EMDR treatment for depression works by targeting the memory networks that fuel depressive symptoms—not the symptoms themselves.
Step-by-Step: What EMDR Therapy Involves
EMDR uses an eight-phase model:
- History-taking & case formulation
- Preparation & stabilization
- Assessment of the target memory
- Desensitization (bilateral stimulation)
- Installation of positive belief
- Body scan
- Closure
- Re-evaluation
This sequence ensures safety, pacing, and integrated processing without flooding or overwhelm.
EMDR DeprEnd Protocol (High-Level Overview)
The DeprEnd protocol—used in several EMDR depression studies—focuses on:
- Past experiences linked to depressive beliefs
- Current triggers
- Future vulnerability (relapse themes)
No procedural details are given here, but the protocol has shown promising outcomes in major depressive disorder when trauma or adverse life experiences are part of the clinical picture.
What Research Says About EMDR for Depression
Early Feasibility Studies (N ≈ 13)
Small pilot studies reported:
- Significant reductions on Hamilton Depression Rating Scale (HRSD)
- Improvements on PHQ-9 and BDI-II
- Faster symptom reduction than expected in traditional therapy alone
Caveat: small samples, inconsistent follow-up, heterogeneous depression types.
Larger Naturalistic Studies (N = 49)
One frequently cited naturalistic study found:
- ~50% achieved remission by discharge
- 74% remained depression-free at 12-month follow-up (Frontiers in Psychology, 2022)
- People with trauma histories often responded more quickly and more completely
- Those without trauma still benefited, but with greater variability
Controlled Trials & Meta-Analyses
Key findings across RCTs:
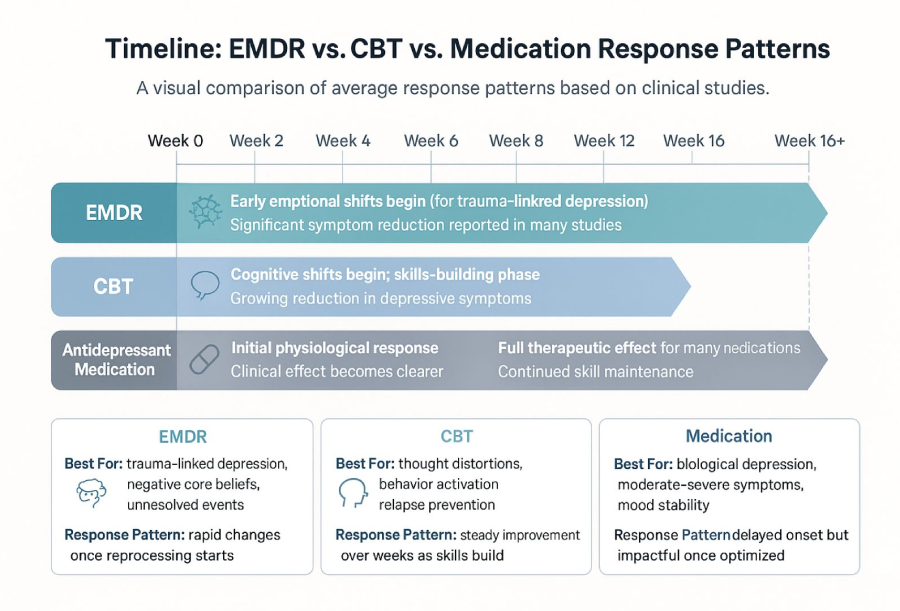
- EMDR was comparable or superior to CBT for some patients
- Many achieved remission in 6–8 EMDR sessions
- EMDR was rated less emotionally taxing by participants
- Symptom improvements often persisted beyond 3–12 months
Key Takeaways Without Overclaiming
- Yes, EMDR helps with depression, especially trauma-linked depression.
- No, EMDR is not a universal depression cure.
- It works best when depressive symptoms originate from past experiences that remain unprocessed.
- For biologically driven depression, EMDR may be supportive—but not sufficient as a standalone.
When EMDR Helps Most With Depression
Major Depressive Disorder (MDD) Linked to Trauma
Common contributing themes:
- Childhood emotional abuse or neglect
- Losses, separations, attachment injuries
- Chronic criticism or shame-based environments
Recurrent or Long-Term Depression
EMDR can help when traditional therapy improves skills but not the underlying emotional wound.
Reactive Depression
Triggered by:
- Divorce
- Job loss
- Medical diagnosis
- Traumatic accidents
- Sudden life changes
EMDR reduces the emotional “charge” around the precipitating event.
Postpartum Depression (High-Level)
EMDR may assist with:
- Traumatic birth experiences
- Emergency medical interventions
- Infant loss
- Fear-based memories from pregnancy
It does not treat hormonal causes but may relieve associated trauma.
Seasonal Affective Disorder (SAD)
SAD is biologically driven, but EMDR may help if:
- Specific life-period memories worsen during certain seasons
- Grief anniversaries or trauma triggers coincide
- Negative self-beliefs amplify winter episodes
When EMDR May Be Less Effective
Depression Not Linked to Adverse Experiences
If no traumatic or distressing formative events are present, EMDR may have limited impact.
Highly Biological or Mood-Cycle-Driven Depression
Examples:
- Bipolar depression
- Melancholic subtype
- Endocrine or hormonal depression
- Seasonal neurobiological depression
EMDR may assist with associated stress but not core mood cycling.
When Stabilization Needs to Occur First
- Acute crises or suicidality
- Severe dissociation
- Unmanaged substance use
- Untreated medical contributors
EMDR requires readiness and stability.
So, Does EMDR Work for Depression? A Balanced View
What “Working” Means in Research
Measured outcomes include:
- Reduced PHQ-9 or BDI-II scores
- Better emotional regulation
- Less reactivity to triggering memories
- Improved daily functioning
Why Results Vary
- Trauma load
- Memory storage differences
- Cognitive reactivity
- Therapist skill
- Treatment pacing
- Patient readiness
The Role of Therapist Skill
EMDR is not plug-and-play.
A good clinician ensures:
- Correct target selection
- Appropriate pacing
- Proper stabilization
- Safe closure
- Integration between sessions
EMDR vs. Other Non-Pharmacological Treatments for Depression
How EMDR Differs From CBT, ACT, IPT
- CBT: challenges current thoughts
- ACT: focuses on values & acceptance
- IPT: emphasizes relationships
- EMDR: targets the root memory network driving the beliefs
How EMDR Fits Into a Broader Care Plan
Often integrated with:
- Medication
- CBT or ACT
- Lifestyle changes
- Sleep interventions
- Medical evaluation
Where EMDR Complements Medication
Medication regulates mood.
EMDR rewires experiential memory.
The two approaches can work together.
EMDR Protocols Used in Depression Work (High-Level)
Standard EMDR Protocol
Targets:
- Past events
- Present triggers
- Future fears
DeprEnd Protocol
Designed for depressive symptoms rooted in specific experiences.
Targeting Negative Beliefs and Emotional Blocks
Focuses on:
- Worthlessness
- Helplessness
- Shame
- Self-blame
Can EMDR Make Depression Worse?
Temporary Distress Is Possible
Processing difficult memories can briefly intensify mood.
Underlying Factors Include:
- Insufficient preparation
- High emotional volatility
- Complex trauma
- Identity-based shame
Why Temporary Spikes Aren’t “Harm”
Many EMDR studies document short-term symptom activation that resolves as the memory network integrates.
What People Ask Before Starting EMDR for Depression
- How do I know if my depression has trauma roots?
- Will EMDR bring up memories I don’t want to revisit?
- How long does EMDR for depression take?
- What if my depression is episodic?
- What if therapy and medication didn’t help?
Practical Considerations Before Trying EMDR
- A thorough assessment matters more than any protocol.
- Stabilization skills are required in advance.
- Set realistic expectations—processing is a journey, not a switch.
- Track progress through daily functioning, not mood alone.
Final Thoughts: What EMDR Can and Cannot Do for Depression
EMDR is not a miracle cure.
It’s not a substitute for medication in biologically driven depression.
And it won’t fix every depressive episode.
But for people whose depression is shaped by unresolved memories, negative self-beliefs, or long-standing emotional wounds, EMDR can be transformative—often in fewer sessions than traditional therapy.
The real key is personalization: the right therapist, the right timing, and the right targets.