EMDR For PTSD
Dec 12th 2025
If you’re searching for EMDR for PTSD, you’re probably caught between two questions:
Does EMDR really work — and is it right for me?
This guide answers both with a level of clarity, depth, and evidence missing from most online articles. It merges insights from the VA, DoD, APA, major meta-analyses, and decades of clinical research — all distilled into a single, authoritative resource.
By the end, you’ll understand:
- What EMDR therapy for PTSD actually is (without the fluff)
- How EMDR works in the brain
- Whether EMDR is effective for complex PTSD (CPTSD)
- How many EMDR sessions are typically needed
- What happens in an EMDR session
- Who benefits most and who may need an alternative
- What the science actually says vs. what marketing says
And you’ll walk away with a grounded, expert-level understanding of this trauma treatment - not the oversimplified version you see everywhere else.
What Is EMDR Therapy for PTSD?
Eye Movement Desensitization and Reprocessing (EMDR) is a trauma-focused psychotherapy developed by Dr. Francine Shapiro in the late 1980s. It’s now recognized internationally as one of the most effective treatments for post-traumatic stress disorder.[1]
Unlike talk therapy, EMDR:
- Does not require you to describe your trauma in detail
- Does not require homework
- Works by reprocessing stored traumatic memories, not by talking about them
Authoritative bodies that recommend EMDR for PTSD include:
- VA/DoD Clinical Practice Guidelines (2023) - “Strong For” recommendation [2]
- World Health Organization (WHO) [3]
- National Institute for Health and Care Excellence (NICE, UK) [4]
- American Psychological Association (APA) - conditional recommendation as a second-line but evidence-supported treatment [5]
Why this matters: EMDR is not fringe or experimental. It is an established, evidence-backed treatment used globally in trauma centers, VA clinics, and private practices.
How Does EMDR Work for PTSD?
To understand EMDR therapy for trauma and PTSD, here’s what researchers agree on:
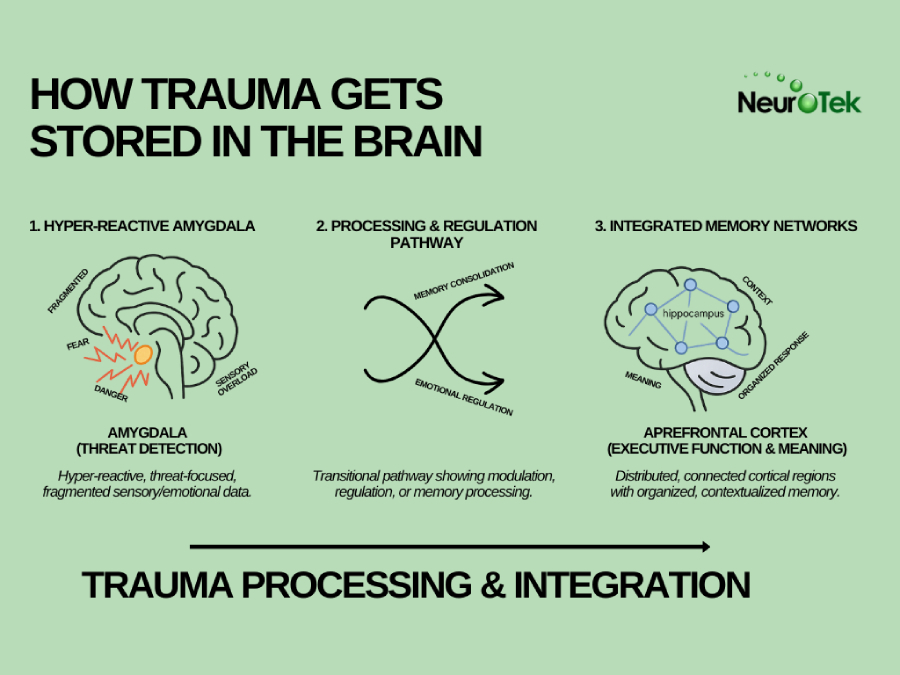
PTSD forms when traumatic memories don’t get fully processed.
During trauma, the brain’s stress-response system becomes overwhelmed, preventing the memory from integrating normally. Instead of being stored as a past event, the memory becomes “stuck” and remains activated as if the danger is still happening.[6]
The memory becomes embedded with:
- intense emotions, which stay locked into the memory and can be triggered long after the event is over.
- distorted beliefs, such as “It was my fault” or “I’m not safe,” which often develop because the brain is trying to make sense of overwhelming events.
- physical sensations, which the nervous system continues to associate with danger, causing the body to react even when the person is safe.
- vivid sensory fragments, like images, sounds, or smells, which often reappear involuntarily because they were encoded under extreme stress.
This leads to symptoms such as:
- flashbacks, where the person momentarily relives the trauma as if it is happening again.
- intrusive memories, which push into awareness without warning and disrupt daily functioning.
- hypervigilance, a constant state of scanning for danger because the brain believes the threat has not passed.
- nightmares, which reflect the brain’s ongoing attempts to process trauma during sleep.
- emotional numbing, where the nervous system shuts down feelings because they feel too overwhelming to manage.
- avoidance, a coping strategy where the person tries to stay away from reminders of the trauma because they trigger intense distress.
EMDR stimulates the brain’s natural processing system.
A typical EMDR session involves:
- recalling a part of the trauma
- focusing on the negative belief associated with it
- noticing related body sensations
- engaging in bilateral stimulation (BLS) through eye movements, tones, or tapping
Researchers believe the back-and-forth stimulation helps the brain access the memory network and reprocess it the way it should have originally.
Authoritative research shows:
- moderate to large reductions in PTSD symptoms
- reductions in depression and anxiety
- improvements maintained long-term
- EMDR often performs as well or better than CBT and Prolonged Exposure [7]
Important nuance:
There’s debate about whether bilateral stimulation is the key mechanism — but even in studies where the “why” is debated, the clinical outcomes remain strong.
What Happens in EMDR Treatment? The 8-Phase Model Explained
EMDR therapy follows a standardized 8-phase protocol, which makes it structured, efficient, and predictable.
1. History-Taking & Treatment Planning
Your therapist gathers a detailed understanding of your trauma history, symptoms, and life patterns to identify the most impactful targets for EMDR processing. This may involve mapping out multiple memories, themes, or early life experiences that contribute to your current distress. For individuals with CPTSD or complex trauma, this stage often requires additional time to ensure all relevant memory networks are accurately identified and prioritized.
2. Preparation
During this phase, your therapist teaches grounding skills and emotional regulation strategies to help you stay stable during reprocessing. You may practice breathing exercises, visualization techniques, or containment strategies to ensure you can tolerate difficult emotions when they surface. The goal is to build enough internal resources that EMDR does not feel overwhelming or unsafe as deeper material arises.
3. Assessment
In assessment, you pinpoint the specific traumatic memory or image you will target, along with the negative belief attached to it (such as “I’m powerless” or “I’m in danger”). You also identify the emotions and physical sensations activated by that memory, which helps anchor the experience in the brain’s sensory network. This clarity allows the therapist to measure progress and ensures that reprocessing is focused, intentional, and grounded in what you actually feel.
4. Desensitization
You recall the traumatic event while engaging in bilateral stimulation—eye movements, tapping, or alternating tones—for short, structured intervals. As the sets continue, your distress typically begins to decrease, and previously overwhelming emotions become more tolerable. This happens because the brain is reprocessing the memory, allowing it to lose its emotional “charge” and integrate into long-term storage more adaptively.
5. Installation
Once the distress associated with the memory decreases, your therapist helps you strengthen a positive belief to replace the old negative one. Examples include shifting from “I’m helpless” to “I’m capable” or from “I’m unsafe” to “I’m safe now.” This stage is crucial because lasting trauma recovery isn’t just about reducing pain — it’s also about installing healthier self-perceptions that foster resilience.
6. Body Scan
Trauma often lingers in the body through tension, numbness, heaviness, or other somatic sensations, even after emotions and beliefs shift. The body scan checks whether any physical reactivity remains when recalling the memory and the new positive belief. If sensations persist, additional sets of bilateral stimulation help release the stored tension until the body and mind are aligned in a calmer state.
7. Closure
Every session ends with restoring emotional stability, whether the memory has been fully processed or not. Your therapist may guide you through grounding exercises or visualization techniques to ensure you leave the session feeling centered and safe. This phase reinforces your sense of control and prevents unfinished material from destabilizing you between sessions.
8. Reevaluation
At the beginning of each new session, your therapist reviews how you’ve felt since the last reprocessing and checks whether the targeted memory still carries any distress. They also assess whether new memories, triggers, or insights emerged that may need to be added to the treatment plan. This ensures the therapy remains dynamic, responsive, and aligned with your ongoing progress.

How Many EMDR Sessions for PTSD?
The answer depends entirely on the type, duration, and complexity of the trauma.
Single-event PTSD
Single-event PTSD (for example, a car accident or isolated assault) often requires fewer sessions, and a range of 6–12 sessions is typical. Many studies even show noticeable improvement within the first 3–4 sessions, especially when the traumatic event is clearly defined and the client has strong baseline stability.
Multiple traumas / childhood trauma / long-term abuse
Multiple traumas, childhood trauma, or long-term abuse require more time because EMDR must work through deeper, more interconnected memory networks.
EMDR for complex PTSD (CPTSD)
EMDR for complex PTSD (CPTSD) requires additional time and care due to:
- fragmented memory networks, which make it harder for the brain to process trauma as a single coherent narrative.
- attachment wounds, which often require stabilization work before direct trauma processing can begin.
- identity-level beliefs, such as “I’m worthless” or “I’m unlovable,” which take longer to shift because they formed over many years.
- dissociation risk, as CPTSD clients are more likely to become overwhelmed or disconnected during reprocessing.
- chronic shame, which can slow progress because clients may struggle to stay compassionate and grounded as difficult memories arise.
For these reasons, the average number of EMDR sessions for CPTSD ranges from 20–60 sessions, depending on the severity of the trauma and the client’s emotional stability.
So… how many EMDR sessions for complex PTSD specifically?
Research and clinical consensus: at least 6 months of weekly treatment, often longer.
This is not a failure — it’s a reflection of the complexity of the trauma.
Does EMDR Work for Complex PTSD?
Short answer: Yes — but with important caveats.
EMDR can be highly effective for CPTSD when the therapist is experienced, when adequate preparation and stabilization are emphasized, and when treatment moves at a gradual, controlled pace. It is also essential that dissociation is carefully monitored and managed throughout the process, since CPTSD clients often have more complex internal dynamics.
However, EMDR may be more challenging when the client has difficulty regulating emotions, when their living environment or relationships are unstable, or when active addiction interferes with the ability to stay present in therapy. Problems may also arise if the therapist moves too quickly or pushes reprocessing before the client is ready, which can lead to overwhelm rather than healing.
The strongest outcomes for CPTSD occur when EMDR is delivered within a phase-based model, beginning with stabilization and skills-building, followed by the EMDR trauma processing itself, and finishing with integration and reconnection work. This structured sequence helps ensure that clients have the internal resources they need before engaging deeply with traumatic memories and that they can successfully integrate the changes that emerge afterward.
Is EMDR More Effective Than CBT or Prolonged Exposure?
Meta-analyses found that EMDR often produces equal or even greater reductions in PTSD symptoms when compared to CBT. The research also shows that EMDR leads to stronger improvements in intrusion and hyperarousal symptoms, which are two of the most persistent and distressing features of PTSD. Additionally, EMDR tends to have lower dropout rates, in part because clients do not have to narrate their trauma in detail, making the process more tolerable for many individuals. [8]
However, there are important nuances. For certain individuals—such as those with psychotic disorders—Prolonged Exposure can outperform EMDR for specific symptoms. Research involving refugees with high instability also suggests that EMDR may offer no significant advantage over stabilization-only treatments, highlighting the importance of context and clinical judgment.
Bottom Line:
EMDR is one of the top-tier, gold-standard PTSD treatments — but not a universal cure-all.
What the Research Says: Evidence Summary
Meta-Analyses (37 RCTs, 1,557 participants)
Meta-analyses covering 37 randomized controlled trials and 1,557 participants show that EMDR leads to moderate-to-large reductions in PTSD symptoms. These reviews also found notable decreases in depression, with effect sizes around g = –0.643, and meaningful reductions in anxiety, with effect sizes around g = –0.640. EMDR produced a strong reduction in subjective distress as well, with an effect size of approximately g = –0.956. The evidence further indicates that EMDR tends to be more effective when administered by therapists with extensive experience and when sessions last longer than 60 minutes.
Randomized Controlled Trials (2014–2017)
Randomized controlled trials conducted between 2014 and 2017 reinforce these findings. EMDR significantly reduced PTSD symptoms in three out of four studies conducted during this period. It outperformed both relaxation therapy and waitlist conditions, demonstrating a clear therapeutic advantage. Among Syrian refugees, EMDR drastically lowered PTSD diagnosis rates, and in patients with multiple sclerosis, 85 percent no longer met PTSD criteria after completing treatment. However, in some refugee populations with severe instability, EMDR did not outperform stabilization-only approaches, showing that context and patient readiness remain key factors. [9]
What Does This Mean for Real-World Clients?
For real-world clients, this research means that:
- EMDR works - often quickly
- EMDR is culturally adaptable
- EMDR is safe and well-tolerated
- EMDR is most effective when performed by highly trained clinicians
Who Can Benefit From EMDR for PTSD?
Many people can benefit from EMDR, including:
- people with single-event trauma
- patients with childhood trauma who can tolerate emotional activation
- veterans
- survivors of violence or accidents
- people who don’t want to recount trauma verbally
- individuals who plateaued in talk therapy
May require modifications or longer preparation:
- CPTSD
- dissociation or depersonalization
- unstable housing or relationships
- individuals with limited emotional regulation
- psychotic disorders (mixed research outcomes)
What Are the Risks of EMDR?
EMDR is safe, but it is not always gentle. Because it works directly with traumatic memory networks, it can temporarily intensify emotions before relief sets in.
You may experience:
- a temporary rise in distress, especially during early sessions when the brain is first beginning to activate and process traumatic material.
- emotional flooding, where strong feelings surface more quickly than expected as the nervous system starts releasing long-held tension.
- vivid dreams, which often occur because the brain continues processing memories between sessions, much like an intensified REM cycle.
- fatigue, as trauma reprocessing can be mentally and physically taxing, similar to the exhaustion people feel after intense emotional work.
- the surfacing of previously repressed memories, which can happen when blocked or fragmented trauma networks finally connect and integrate.
In competent hands, these effects are:
- expected, because temporary discomfort is a normal part of reorganizing traumatic memory networks.
- normal, reflecting the brain’s natural healing process rather than a sign that anything is going wrong.
- manageable, especially when the therapist uses proper pacing, grounding techniques, and stabilization strategies.
- transient, typically fading as treatment progresses and the traumatic material loses its emotional intensity.
Most clients report substantial relief by the end of treatment, even if the early phases feel intense or unfamiliar.
EMDR vs. Other PTSD Treatments: When EMDR Is the Best Choice
|
Treatment |
Best For | Limitations |
| EMDR | PTSD, CPTSD, clients who avoid talking about trauma | Requires skilled therapist; emotional intensity |
| Prolonged Exposure (PE) | Fear-based PTSD, veterans | High dropout rate; requires detailed trauma narration |
| Cognitive Processing Therapy (CPT) | Shame, guilt, self-blame | Heavy cognitive work |
| Trauma-Focused CBT | Broad trauma reactions | Requires homework; slower change |
When EMDR is ideal:
You want fast, structured treatment without extensive verbalization.
Conclusion: Is EMDR Worth Trying for PTSD?
If you’re dealing with PTSD or the long shadow of complex trauma, EMDR is one of the most effective, research-backed treatments available today.
The evidence is clear:
- It works for PTSD.
- It often works for CPTSD.
- It reduces symptoms quickly.
- It doesn’t require retelling your trauma.
- It’s recommended by the world’s top clinical authorities.
If you found this guide helpful, share it - someone else searching for clarity about PTSD treatment may need it just as much as you do.
Sources
[1] EMDR Institute, Inc.- What is EMDR Therapy?
https://www.emdr.com/what-is-emdr/
[2] VA/DoD Clinical Practice Guidelines (2023) - PTSD: National Center for PTSD.
https://www.ptsd.va.gov/professional/treat/txessentials/cpg_ptsd_management.asp
[3] World Health Organization (WHO) - Post-traumatic stress disorder.
https://www.who.int/news-room/fact-sheets/detail/post-traumatic-stress-disorder
[4] National Institute for Health and Care Excellence (NICE, UK) - Post-traumatic stress disorder.
PMC - PubMed Central - Post-traumatic stress disorder: what does NICE guidance mean for primary care?
https://pmc.ncbi.nlm.nih.gov/articles/PMC6592320/
https://www.nice.org.uk/guidance/ng116
[5] American Psychological Association (APA) - Clinical Practice Guidelines for the Treatment of Posttraumatic Stress Disorder.
https://www.apa.org/ptsd-guideline/treatments/eye-movement-reprocessing
[6] referenced in the book Light in the Heart of Darkness: EMDR and the Treatment of War and Terrorism Survivors by clinical psychologist Steven Silver, PhD.
[7] National Library of Medicine - Efficacy of eye-movement desensitization and reprocessing for patients with posttraumatic-stress disorder: a meta-analysis of randomized controlled trials.
https://pubmed.ncbi.nlm.nih.gov/25101684/
[8] Efficacy of Eye-Movement Desensitization and Reprocessing for Patients with Posttraumatic-Stress Disorder: A Meta-Analysis of Randomized Controlled Trials
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0103676
[9] National Library of Medicine - An Analysis of Contemporary Oncology Randomized Clinical Trials From Low/Middle-Income vs High-Income Countries